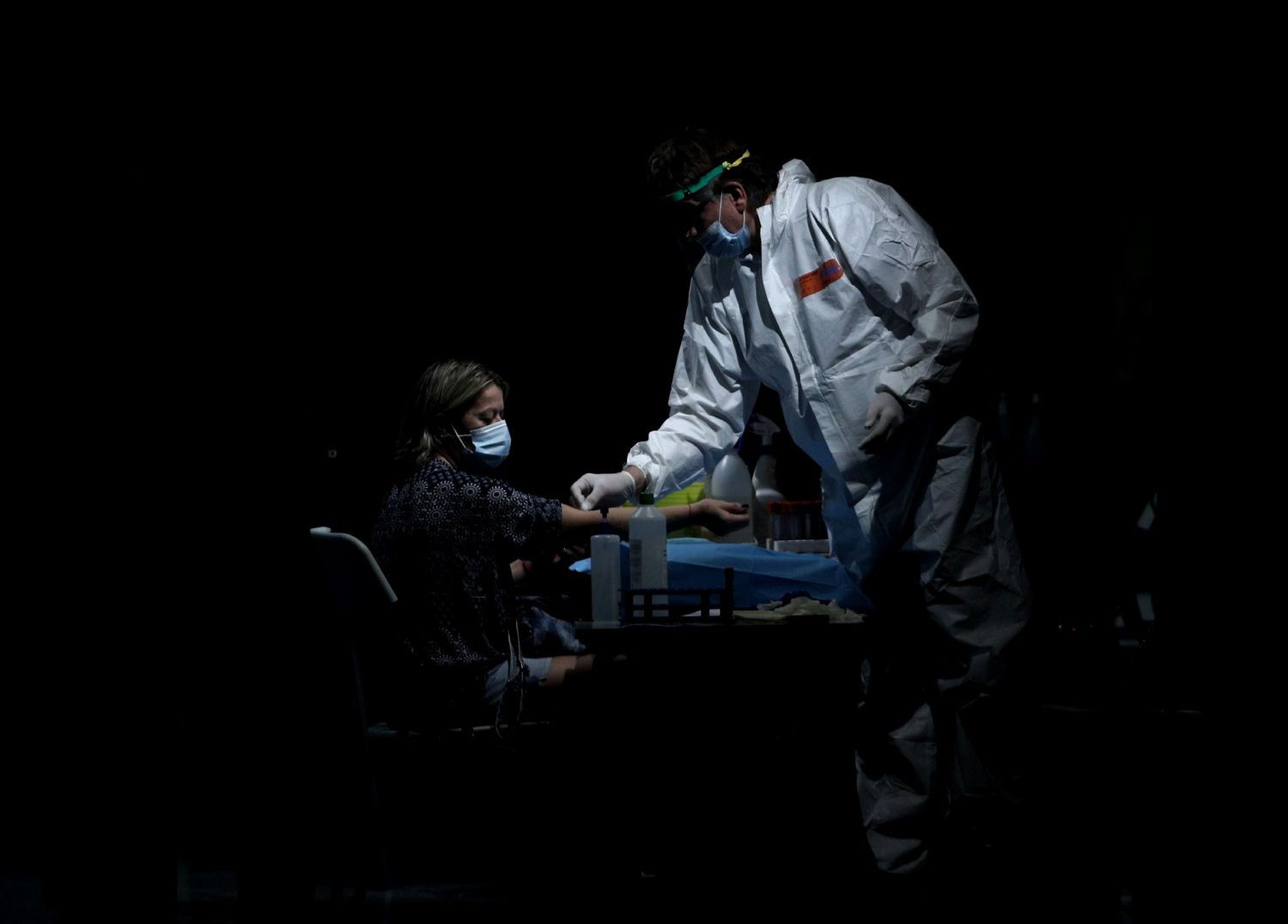
The blood of thousands of people has just brought good news on one of the most crucial fronts in the war against the new coronavirus: natural immunity.
Since the beginning of the pandemic, one of the most pressing questions has been how effective is the immunity that a person has after overcoming the infection and, above all, how long does it last. It is an agonizing question because to answer it you have to wait, despite the pandemic urgency. The same happened with SARS in 2002: at first it was doubted that there would be lasting immunity. We now know that the people who passed the virus still had antibodies 12 years later.
In recent days there have been reports of a few people reinfected by SARS-CoV-2 , including some who have suffered a more serious illness the second time. Antibodies are proteins of the immune system that bind to the virus and prevent it from infecting more cells. Several studies from months ago showed that antibodies decline within a few months of infection in people with mild disease, including the serological study that was carried out in Spain. So are those that overcome the first infection protected?
Based on data from one of the largest studies to date on this topic, the most likely is yes; And that antibody-mediated protection lasts for at least seven months.
“Our study shows that it is possible to generate lasting immunity against this virus”, explains Deepta Bhattacharya, a researcher at the Cancer Center of the University of Arizona (USA) and co-author of the work, which will be published in the journal Immunity . “In moderate infections that we have analyzed, the antibody response seems quite conventional; the levels of these proteins go up at first and then go down, but then they stabilize ”, he adds. Reinfections, he warns, are “exceptional” cases.
When SARS-CoV-2 enters our body, a complex response of the immune system begins that takes about two weeks to complete and involves millions of cells throughout the body. Some of them are extremely sophisticated : they can forever remember a pathogen and develop the molecular weapons to destroy it, including different types of high-potency antibodies.
The Arizona study stems from a massive testing campaign involving 30,000 people. The study has focused on the data of almost 6,000 of them and has analyzed the production of neutralizing antibodies in more than 1,000.
The prevalence of infections is low, with only about 200 people found to have passed the infection and produced neutralizing antibodies, Bhattacharya explains . The most that the team has managed to go back in time to see how long the antibodies last is those seven months, since the coronavirus epidemic arrived relatively late in this state. “We have only been able to test six people who were infected between five and seven months ago, but we have many more who did between three and five months ago. We don’t have a crystal ball to know how long antibodies last, but based on what we know about other coronaviruses, we expect the immune response to be sustained for at least a year and probably much longer, ”explains Bhattacharya.
The US team believes that previous data pointing to antibodies falling early is due to the analysis of a type of blood plasma cells that are the first to come after an infection, but have a short life. These are cells capable of secreting not very specific antibodies, such as IgM. Some time later, a second type of longer-lived blood cells comes into play that go to the germ centers, a kind of headquarters of immunity located in the ganglia and spleen where they receive antigens from the new virus that allow them to identify it with much more precision and develop much more specific antibodies, the famous IgG.
Among this second wave of antibodies is an elite troop directed against the protein that differentiates the new coronavirus from others of its kind: the spicule. This spike-shaped protrusion that protrudes from its envelope is responsible for fitting into the receptor of human cells to open them , take over their biological machinery and begin to reproduce without restraint. This is the beginning of an infection, with or without symptoms. In a minority of cases , the entry of the virus generates a disproportionate response from the immune system that can end up causing death.
The Arizona team has analyzed two of these antibodies capable of binding to different regions of the spike and thus blocking their entry into cells. This type of antibody has been shown in the laboratory to be able to stop the spread of the virus in a much more effective way than those that attack the protein N – nucleocapsid – located inside the pathogen in order to protect its genome and facilitate its copying. once it has entered the cell.
In Spain, the serological study showed that antibodies against the coronavirus declined about three months after infection in four out of ten infected with mild symptoms. The same happened in other studies in other countries. The problem, the US researchers now argue, is that these studies measured only antibodies against protein N. In their work they show that antibodies against the spike and the part of it that comes into contact with human cells (RBD) are much more durable.
The absence of this type of durable antibody may explain the fatal cases of Covid-19, according to a recent study coordinated by two of the best hospitals in Boston (USA). Patients who end up dying do not generate germ bodies, and therefore fail to produce specialized neutralizing antibodies, as shown by the analysis of 17 very severe covid patients, including 11 deceased whose spleens and lymph nodes were analyzed at autopsies. Without this elite troop, the immune response is twisted and the body begins to generate a cascade of inflammatory proteins that end up producing a fatal outcome.
These findings have important implications for the effectiveness of vaccines. Most of the more advanced ones are based on generating immunity against various